The use of CRITICAL THINKING skills during assessment to determine hemodynamic status.
First glance, size up the patient... What does inadequate cardiac output look like?
• Think perfusion
In a crisis, physical assessment is brief & focuses on parameters that are key to perfusion: heart rate & rhythm, presence & quality of pulses, capillary refill, color of skin & mucous membranes,
and urine output.
Skin is the first thing one sees while observing a patient. Pallor indicates a decreased perfusion state. The skin becomes pale when blood is shunted to organs. Cyanosis indicates hypoxia; The skin may be cool or warm. Coolness may be an indicator of hypoperfusion. Moisture may occur from perspiration as a result of fever, vasodilation, or work. Edema may be present. This may be from excess IV fluids given to the patient.
One should be thinking about the effects on perfusion (and hemodynamics) when vital signs are abnormal.
• Temperature: hypothermia, hyperthermia
When observing heart rate, keep in mind the normal range of 60-100 beats per minute. When the heart rate is above 100 it may be an indicator of compensation for a low cardiac output.
• Pulse: perfusion, quality, correlation with ECG, SaO2
• Respirations: depth, rate, symmetry, character
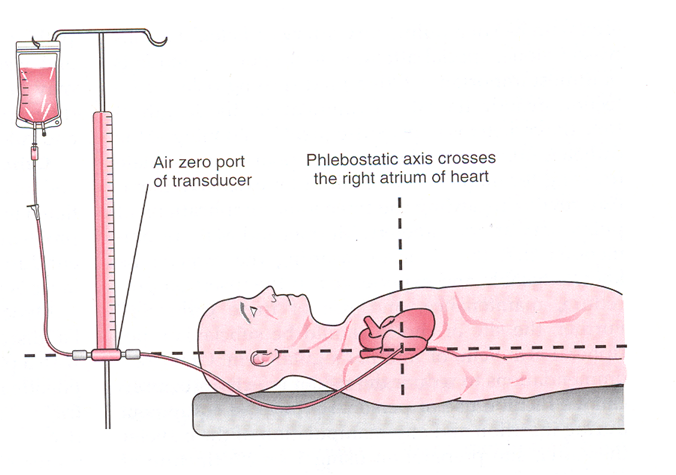
Correlate the arterial blood pressure to the cuff pressure and note the difference, if present. It is not necessary to assess both cuff and arterial pressures at all intervals. It may also be annoying to the patient and painful. Automatic blood pressure should be correlated with an auscultated blood pressure for accuracy especially in cases where the patient is having dysrhythmias. Arterial blood pressure is the most accurate blood pressure, measured directly against the arterial wall. The equipment must be functioning properly and placement correct. The transducer should be placed at the level of the phlebostatic axis. Repositioning of the transducer should occur when the patient is repositioned.
• Blood pressure: hypotension, hypertension
Assess waveform quality for crispness, dampening, and dicrotic notch. Baseline strips should be mounted
• ECG, waveforms
This is the position for all transducers: arterial line, CVP line, PA catheters.
The position is the 4th intercostal space at the midaxillary line. Mark the position on the patient.
Zero the transducer according to the method of the institutional monitoring devices. This negates the effect of atmospheric pressure.
1. Turn the stopcock at the transducer to close the line to the patient and open to atmosphere.
2. Press the zero button to reference monitor. It will read "0"
3.Turn the stopcock at the transducer to close the line to atmosphere and open to the patient
4. Check caps to secure and waveform
.
*Bucher, L. & Melander, S. (1999). Critical Care Nursing