Blood enters the heart from the superior and inferior vena cava into the right atrium, into the right ventricle, into the pulmonary artery, then into the lungs, and back to the heart via the pulmonary vein, into the left atrium, into the left ventricle, through the aorta and out to the body. Preload is the blood that enters the heart either from the vena cava (the body) or the pulmonary vein (lungs).
Preload of the right side of the heart is measured using a central venous catheter to measure central venous pressure (CVP).
• measures volume from the venous system (superior & inferior vena cava entering the right atrium (normal is 0-8)
Preload of the left side of the heart is measured with the use of a pulmonary artery catheter using the wedge pressure measurement (PAWP) or pulmonary artery end-diastolic pressure (PAEDP).
We will be focusing on the use of the CVP measure as preload for the purpose of this discussion.
If the measured CVP is low, the patient may have a low intravascular volume or may have vasodilation from shock or drug therapy. Giving increased IV fluids or blood products may be considered. These treatments should be carefully considered before administration because of potential fluid overload issues. Treatment with IV fluids (crystalloid or colloid) should be based on the patient's symptoms. By increasing the preload the result would indicate increased myocardial performance (increased volume, hence increased stretch).
If the CVP is elevated, this patient may be experiencing fluid overload or heart failure. An increased CVP is also present with cardiac tamponade, pulmonary hypertension, or chronic left ventricular failure. Another correlating symptom may be increased jugular venous distention. Assess vital signs, urine output, and breath sounds. Diuretic therapy may be indicated.
Afterload is the measure of resistance (or impedance) met when the blood enters the vascular bed. Afterload is a calculation that is made when using a pulmonary artery catheter. Since institutions are moving away from invasive monitoring, it is important to recognize and understand signs and symptoms affecting SVR, even without the direct measurement. We will be focusing on the SVR measure as afterload in this discussion.
• Vascular resistance: measurement of resistance (impedance) met from blood entering the arterial bed
• from the left side of the heart (aorta): systemic vascular resistance (SVR)
• from the right side of the heart (pulmonary artery): pulmonary vascular resistance (PVR)
• Increased VR increases myocardial workload and myocardial oxygen consumption
There is an inverse relationship between cardiac output and SVR, which is often compensatory. If cardiac output is low, such as in hemorrhage, SVR will be elevated (vasoconstriction). If cardiac output is high, as in septic shock, SVR will be low (vasodilation).
In an anemic state, the patient may have compensatory tachycardia because of bleeding or decreased oxygen carrying capacity, and elevated SVR.
When aortic regurgitation is present, the back flow of blood causes an increased cardiac output and lower SVR
In fever and septic shock states, the patient has a very dilated vascular bed. This state would cause an increased cardiac output because there is low resistance to flow. In the case of septic shock the patient is "hyperdynamic" and cardiac output will be abnormally high, and SVR will be abnormally low to extremes.
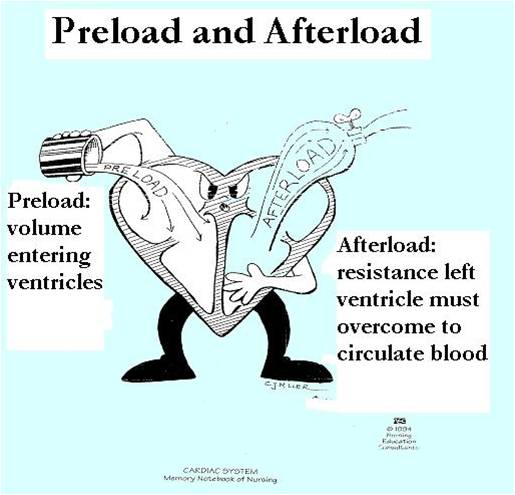
This diagram represents the relationship of preload and afterload. The character here is pouring fluid into the right side of the heart (preload). The left ventricle is ejecting blood into the aorta. The presence of the "spigot" demonstrates that afterload can be high, opening is narrow or nearly closed, making it difficult for fluid to be released; or it is wide open and fluid can pour in freely.
• Force of ventricular ejection
• Refers to pressure generated by ventricles and amount of blood ejected
• Influenced by changes in preload, afterload, and ventricular performance
Contractility cannot be directly measured, even with invasive lines.